-
Cancer
Sharing Mayo Clinic: Slaying the dragon of pancreatic cancer
Thomas Hoffman of Spearfish, South Dakota, was 56 years old, weighed 235, and had been diagnosed with prediabetes when he began to diet. As the pounds melted away, his wife became alarmed at his rapid weight loss. Then one morning, he awoke and his wife told him he was completely yellow — not from the sun streaming into the bedroom, but from jaundice. Thomas went to a local emergency room.
“The doctor comes in and gives us the news: ‘You have pancreatic cancer. You’ve got six months to live. Get your stuff together,’” Thomas says. “What do you do?”
 What his doctors did was send Thomas to Mayo Clinic’s Rochester campus, where he met Mark Truty, M.D., a surgical oncologist, who is rewriting the protocol for treating stage III pancreatic cancer, with notable success. Dr. Truty started Thomas on chemotherapy right away, followed by radiation therapy and then an extensive surgery. After that came more chemo. Now, nearly three years after his diagnosis, Thomas remains cancer-free.
What his doctors did was send Thomas to Mayo Clinic’s Rochester campus, where he met Mark Truty, M.D., a surgical oncologist, who is rewriting the protocol for treating stage III pancreatic cancer, with notable success. Dr. Truty started Thomas on chemotherapy right away, followed by radiation therapy and then an extensive surgery. After that came more chemo. Now, nearly three years after his diagnosis, Thomas remains cancer-free.
“I’ve gained my strength back where I can ride my Harley again,” Thomas says. “I’m never going to be 100 percent. But hey, I’ll live with whatever it takes. I just want to be as normal as I can. I can do my little hobbies. I can help my son out. I can see my grandkids. I help my wife in her business. I just do what I do.”
Thomas is one of more than 100 patients diagnosed with stage III pancreatic cancer who may not have been given a chance elsewhere but have been offered new treatment possibilities at Mayo Clinic, courtesy of a unique approach to this much-feared disease developed by Dr. Truty and his colleagues.
Changing the mentality
In 2016, about 53,000 patients in the United States were diagnosed with cancer of the pancreas, according to the National Cancer Institute. It ranks as about the 10th most common cancer, but the third most deadly. By 2020, it likely will surpass breast and colorectal cancer and be the second leading cause of cancer death in the U.S. Currently, only 7 percent of those diagnosed with pancreatic cancer live more than five years after diagnosis.
Dr. Truty has pioneered a radical new protocol for treatment of the disease, starting with treatment using new cancer drugs and radiation therapy, then followed by marathon surgeries that are rarely tried in conventional treatment.
“We’re trying to change the mentality,” Dr. Truty says. “We have new drugs, and now we’re trying to attach those new drugs to more aggressive operations that doctors have previously denied patients.”
“I want people to talk about it — ‘Yes, I have pancreas cancer. What are my options?’ They’re significantly better now than they were even five years ago.” — Dr. Mark Truty
Data on more than 100 of Dr. Truty’s patients show remarkable success, especially among those who, using conventional criteria, would have been told that surgery was not an option.
“People get that diagnosis, and they hide. They look on the Internet or they’re aware of the disease, and they don’t tell anyone, because there’s such a bad association with it,” Dr. Truty says. “I want people to talk about it — ‘Yes, I have pancreas cancer. What are my options?’ They’re significantly better now than they were even five years ago.”
Deadly spread
Pancreatic cancer is so often lethal because it spreads long before symptoms appear. And at this time, there’s no reliable way to predict who will get pancreatic cancer or who should be tested for it.
For decades, people with this disease have been offered the same treatment. In a small fraction of patients, a surgeon removed the tumor. Chemotherapy then followed surgery if the patient was able to recover from the operation well enough to tolerate it. If the tumor couldn’t be removed with surgery, the patient received chemotherapy alone.
But that approach fails in several ways. First, an operation alone for pancreatic cancer is of minimal benefit. All patients with pancreatic cancer need chemotherapy, and chemotherapy drugs have until recently been largely ineffective. Second, surgery does no good if the tumor has already spread. Or if cancer cells at the margin of the tumor remain behind and later spread.
“Basically, for the last 30 years we’ve had the same practice across the country — across the planet — and we’ve had no incremental improvement in outcome,” Dr. Truty says.
“Half of my practice is patients who have been deemed unresectable after being seen elsewhere. These are patients that have been told they have no hope.” —Dr. Mark Truty
Dr. Truty was particularly interested in the 35 percent of stage III pancreatic cancer patients who show no signs of metastasis but are not considered for surgery because the tumor involves too many veins, arteries and other tissues. They are usually given chemotherapy alone, and survival frequently is less than a year.
“I thought, boy, if we could even get half of them through our chemotherapy-radiation regimen and somehow treat them surgically, we’d be doubling the current number of patients that we could potentially treat,” Dr. Truty says.
He has a personal interest in trying to improve outcomes.
“My father had pancreas cancer,” he says. “He went through the traditional approach. He went to the operating room, had major complications, never got chemotherapy, and died in my arms six months later. I see that same thing occur 25 years later, over and over and over. We keep doing the same thing and hope for a different result.”
Because his father had pancreatic cancer, Dr. Truty himself has an elevated risk. “So I have a vested interest in this as well.”
New tactics
The first step in improving cancer treatment, Dr. Truty decided, was switching to more effective chemotherapy drugs. He settled primarily on two regimens: FOLFIRINOX and gemcitabine-nab-paclitaxel. They are multi-drug combinations shown in New England Journal of Medicine studies in 2011 and 2013 to be far more effective than older drugs.
Dr. Truty also decided to prescribe his patients chemotherapy right away, rather than as a follow-up to surgery. That way, the drugs would have a chance to shrink the tumor and hunt down cancer cells that had spread far away from the pancreas. Moreover, the four months or so of chemotherapy allowed his patients to get in better shape.
“We put them through physical therapy, meet with the nutritionist, the dietitians,” he says. “We get their symptoms under control, and then they go into the operation in significantly better shape to tolerate that procedure, both physically and psychologically.”
Dr. Truty follows chemotherapy with radiation therapy, primarily to kill cancer cells at the site of the operation. That allows him to perform much more aggressive operations than were previously possible. If there’s still no sign the cancer has spread, and the patient’s strength holds out, Dr. Truty performs surgery, including extensive procedures that few other doctors attempt.
“Half of my practice is patients who have been deemed unresectable after being seen elsewhere,” he says. “These are patients that have been told they have no hope. We’re now doing complex vascular resections, both of the veins that supply and drain the intestines and liver, as well tumors involving critical arteries.”
“People aren’t working independently. It’s a whole team approach. That’s how this institution originated.” — Dr. Mark Truty
Dr. Truty’s prep begins the night before surgery. He reviews the operation with the other surgeons who will be involved and looks at models printed from CT scans on 3D printers. The result is a nearly exact replica of the patient’s organs and tumor.
“It’s challenging because every tumor is in a different location. Each tumor involves different blood vessels,” he says. “There’s no textbook for how to do these operations.”
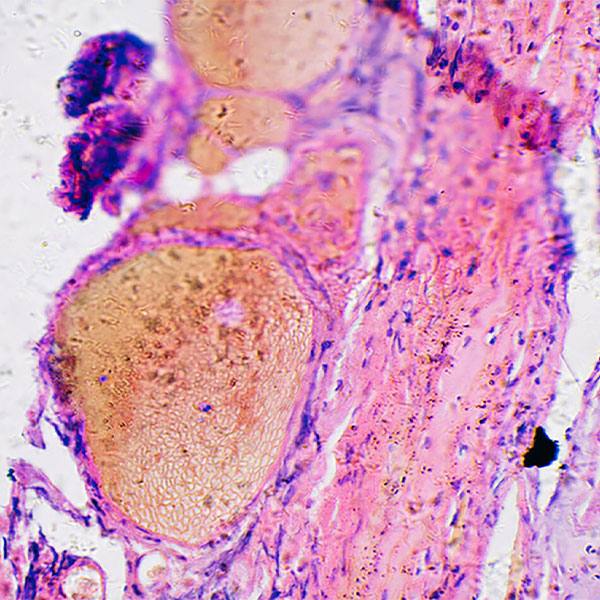
The surgeries are marathon sessions, lasting up to 14 hours. During the procedure, Dr. Truty sends tumor samples to a pathologist who quick-freezes the tissue, slices it and examines it for cancer — a technique developed at Mayo Clinic.
“They go through it slice by slice. They look into the microscope, and they tell us how much tumor is still alive,” Dr. Truty says. “The pathologist will stay till 2 in the morning with me. The greatest excitement for me is when the pathologist says there’s hardly any tumor left alive.”
After surgery, Dr. Truty finishes with an additional round of chemotherapy. Each component of the therapy has a specific purpose. The result is a program that appears to be providing a genuine opportunity to cure pancreatic cancer.
The goal: a cure
Nearly three-and-a-half years ago, Richard Hanson of Lakeville, Minnesota, felt what seemed like a gas bubble in his lower abdomen that wouldn’t go away. He visited his doctor, got a CT scan and MRI, and within a week received a diagnosis of pancreatic cancer. His doctor called Mayo Clinic, and a day later Richard met with Dr. Truty.
Richard underwent the regimen of chemo, radiation and surgery. As he was about enter the operating room, Richard recalls Dr. Truty telling him, “Listen, I told you three to five years, but when I do surgery now, it’s for the cure.”
Dr. Truty removed part of Richard’s pancreas, 15 lymph nodes and his spleen. After that, Richard had a final round of chemo. Nearly three-and-a-half years after his diagnosis, he is showing no signs of recurrence. In fact, he has been golfing regularly for the last two years.
“I finally got out onto the golf course and started swinging a club, and that was really good therapy,” he says.
Richard is one of more than 100 patients Dr. Truty has treated over four years who make up a cohort for a study he plans to publish soon. All had stage III pancreatic cancer with large, entwined tumors that most surgeons would not consider trying to remove. All were treated with extensive chemotherapy, radiation, surgery, and more chemotherapy in certain cases.
With conventional treatment, the expected median survival for these individuals would be less than a year. But with this group, the median survival is over 50 months and counting. The majority of patients show no signs of cancer. Dr. Truty anticipates that perhaps 40 percent will be alive five years after treatment.
“They are potentially cured, which is a word that we seldom use with these patients,” he says.
The promise of research
Dr. Truty believes greater gains are possible. The first step is finding more effective chemotherapy drugs. To do that, Dr. Truty is looking for better scientific models that represent the actual patient.
In his role as a researcher, Dr. Truty is growing tumors from human pancreatic cancer tissues in lab mice with weakened immune systems. These tumors are derived from the very patients he operates on. Because the tumors are virtually indistinguishable from the tumors in the original patients, they provide ideal targets for drug testing. The mice also provide a way to identify protein biomarkers produced by the cancer tumors. The markers may someday be used to screen patients for cancer, as well as to determine which patients will response to specific chemotherapy regimens.
Growing tumors in mice can predict the recurrence of cancer in humans. Cancerous tissue taken from a particular patient — after chemo, radiation and surgery — is transplanted into a mouse to determine if the cancer cells were completely killed or if they are likely to return. If the cancer cells grow in the mouse, that’s an ominous sign.
“I don’t care what you’ve been told elsewhere. Come here and get another opinion. Because we have made significant improvements. We have data that people are living significantly longer.” — Dr. Mark Truty
But, says Dr. Truty, “This also gives us lead time to intervene when the tumor is still microscopic.”
Mayo Clinic is uniquely situated to support Dr. Truty’s brand of aggressive treatment and tumor research. First, many people diagnosed with pancreatic cancer come to Mayo Clinic. That provides an opportunity to develop and refine effective treatment. It also provides many variations of tumors for research. Second, Mayo Clinic’s structure allows easy collaboration between researchers, oncologists, surgeons and pathologists.
“People aren’t working independently,” Dr. Truty says. “It’s a whole team approach. That’s how this institution originated.”
In Dr. Truty’s office hangs a print of St. George slaying the dragon. This image is also Dr. Truty’s door card, which hangs on his patients’ hospital rooms after surgery. The writhing dragon represents cancer and looks a lot like a pancreas. Yet as much as cancer, Dr. Truty is also trying to slay pessimism. He hopes that someday soon, pancreatic cancer will be treated as a chronic disease and not a death sentence.
“I don’t care what you’ve been told elsewhere. Come here and get another opinion,” he says. “Because we have made significant improvements. We have data that people are living significantly longer.”
HELPFUL LINKS
- Learn more about pancreatic cancer.
- Read about Truty’s research.
- Explore Mayo Clinic’s Rochester campus.
- Request an appointment.