-
Sharing Mayo Clinic
3D Printing Paves the Way for Precision Surgeries
The surgical teams assembled to operate on Mayo Clinic's most complex patients lately have begun to consist of more than living, breathing members. The new recruits are usually small enough to hold in your hand, and they don't say a word. But the information conveyed by these 3D anatomical printed models is helping surgeons plan and navigate the trickiest of procedures.
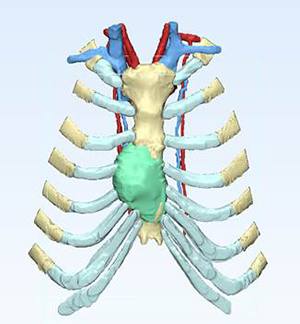
In late 2016, Mayo Clinic thoracic surgeon Mark Allen, M.D. was part of a surgical team that used a 3D printed model to help them prepare to remove a rare, intrusive pancoast tumor. The tumor had grown in the chest of a patient, between his ribs and among the vessels just above his lungs.
By demonstrating precisely where the tumor was in the body, and its proximity to neighboring structures, the 3D model permitted Dr. Allen to remove the tumor in a way that preserved the surrounding vessels and facilitated a successful reconstruction of the patient's thoracic cavity.
"When you have a 3D model, you can hold it and rotate it around. It gives you all the relationships with everything and where things are located," Dr. Allen says. "Within a millimeter of accuracy, you see the same things you will find internally."
Model patients
 From tumor resections to facial reconstructions and heart surgeries, 3D models take away guesswork and facilitate communication among physicians. The models are created from patients' CT scans at the Anatomical Printing Lab in Mayo Clinic's Department of Radiology.
From tumor resections to facial reconstructions and heart surgeries, 3D models take away guesswork and facilitate communication among physicians. The models are created from patients' CT scans at the Anatomical Printing Lab in Mayo Clinic's Department of Radiology.
"They help us tailor the treatment appropriately to every reconstruction," says Mayo Clinic reconstructive surgeon Basel Sharaf, D.D.S., M.D. "Modeling helps with efficiency. It gives the whole team an opportunity to thoroughly assess the surgical plan and the steps of the procedure that will take place in operating room. It allows us to discuss pertinent anatomical and technical details with other team surgical team members.
"The technology has been commonly used for head and neck and craniofacial patients," Dr. Sharaf adds. "It is exciting to employ it in complex chest wall reconstruction, as well."
"Modeling helps with efficiency. It also gives the whole team an opportunity to thoroughly assess the surgical plan and the steps of the procedure that will take place in operating room." — Basel Sharaf, D.D.S., M.D.
The 3D models are moving beyond bony tissue to soft tissue models. Recently, Dr. Sharaf and his colleague Uldis Bite, M.D. used a 3D model to prepare and plan for a complex facial reconstruction. With the help of Jane Matsumoto, M.D., and Jonathan Morris, M.D., in Mayo Clinic's Department of Radiology, they used the patient's imaging to develop the model.
"There was an asymmetry in the cheek bones and soft tissues of temple area, as well as missing bone between the upper jaw and the rest of the face," Dr. Sharaf says. "We needed to address all of these issues to restore form and function. Models help us understand and plan the configuration and volume of tissues we need to restore the defect and tailor the reconstruction to meet those needs."
Touchable teaching tool
While there are drawbacks to using models — the printing process is slow and can be expensive — the potential they have for improving outcomes is vast.
"At Mayo, we see many patients for complicated procedures or those who have had failed procedures," Dr. Sharaf says. "A lot of times, it's the last chance to get the right procedure done. That's where I see the models being really helpful."
Patients also get a chance to view the 3D models. Seeing an anatomically correct model of their inner structures often gives them a better sense of what's going to happen during surgery. And the teaching value of using models goes far beyond patient education.
"For a teaching hospital, using these models is ideal. 3D printed models are great teaching tools to help educate residents, fellows and medical students to understand the complex anatomy involved and what the procedure is going to entail." — Basel Sharaf, D.D.S., M.D.
"It's always a good thing to work with other people and get different ideas," says Dr. Allen of the collaborative nature of working with a 3D model. And not only do models help physicians learn from one another, they are a valuable tool to educate students.
"For a teaching hospital, using these models is ideal," Dr. Sharaf says. "3D printed models are great teaching tools to help educate residents, fellows and medical students to understand the complex anatomy involved and what the procedure is going to entail."
HELPFUL LINKS
- Learn more about 3D printing at Mayo Clinic.
- Read about Mayo Clinic's Department of Plastic and Reconstructive Surgery.
- Explore the Department of Radiology.
- Schedule an appointment.








