-
Cardiovascular
Sharing Mayo Clinic: A passion for serving underserved communities
Concerned by health disparities in African-American communities, Dr. LaPrincess Brewer developed a program that partners with local churches to foster healthy lifestyle choices and improve heart health.
Editor's note: LaPrincess Brewer, M.D., a Mayo Clinic cardiologist, has been applying an innovative, community-based participatory research model to prevent heart disease in underserved communities. Dr. Brewer's program, called Fostering African-American Improvement in Total Health (FAITH), has been recognized nationally and internationally as making substantial improvements in the health of its participants. This is Dr. Brewer's account of how she got started in medicine and what compels her research.
By LaPrincess Brewer, M.D.
I don't have the classic story, where as a child, I dreamed of being a physician and went around wearing a toy stethoscope and carrying a doctor's bag.
I discovered my love of patient care and medicine after my freshman year at Howard University in Washington, D.C. As a chemical engineering major, I completed a summer internship at 3M in Minnesota. I loved the experience and had a supportive unit supervisor. It was a direct application of all the knowledge I gained in class. But something was missing.
Combining two loves
That palpable void was human touch and having a lasting impact on people's lives. So when I went back to college that fall, I contacted my advisers and told them I wanted to try something that would allow me to interact with people beyond a basic science laboratory. They recommended clinical research as an avenue to shadow a physician balancing clinical practice and research for the benefit of patients. I had never really thought of this as a possibility.
The next summer, I was selected into Research Experiences for Undergraduates — a summer research fellow program at the Duke University School of Medicine in Durham, North Carolina. I fell in love with it.
"To understand why the disparities existed, I wanted to become more equipped to tackle them head on."
LaPrincess Brewer, M.D.
I was assigned as a mentee to a world-renowned cardiologist within the Center for Emerging Cardiovascular Technologies to work on a project in partnership with NASA. The aim of the project was to develop better therapeutic measures to prevent muscle breakdown and dysfunction in astronauts, which is a major limitation to long-term space missions by humans. Having the opportunity to shadow him was eye-opening. I discovered that I could combine my love of science and engineering with patient care. From that moment on, I made it my goal to apply to medical school. I was fortunately accepted into the George Washington School of Medicine & Health Sciences in Washington D.C., and the rest is history.
Losing loved ones to disease
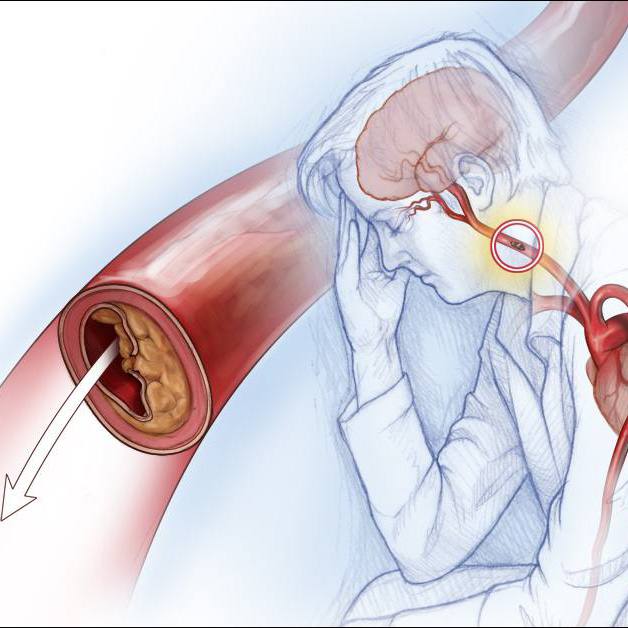
I was really drawn to becoming a physician, given the privilege afforded to care for and learn from patients and then channel this knowledge to have a larger impact on population and public health, particularly within underserved groups. This stems back to my upbringing within the African-American church. I saw so many members of my congregation — many people I looked up to — slipping away from uncontrolled chronic diseases, predominantly heart disease and its risk factors. Not all were related to me, but they all felt like family. I wondered why they were dying so early from conditions that could have been prevented in the first place. There was so much potential loss.
In between my third and fourth year of medical school, I decided to take a year to pursue a master of public health degree, which stemmed from my clinical practice as a medical student. I became overwhelmed with the degree of cardiovascular disease health disparities within the communities we served in our nation's capital. These disparities were magnified among the poor and underserved. To understand why the disparities existed, I wanted to become more equipped to tackle them head on.
Changing the culture of health and wellness
I was honored to be accepted to the Johns Hopkins Bloomberg School of Public Health in Baltimore. One of our elective courses in health promotion charged us with developing a community-based intervention that had the potential to be sustained over the long term. My group members were interested in chronic disease prevention within the African-American community. It was only fitting that we would partner with the African-American church, given its profound impact in the lives of African-Americans from a spiritual, social, political and health standpoint.
We developed the project in partnership with a local African-American church that was a stone's throw from the medical institution. No one had ever reached out to this church to do any sort of health program from Hopkins. And it was perfect timing for us, as the church's pastor had a keen interest in establishing a health ministry within the church. He expressed sorrow in witnessing several of his church members passing way from heart disease, hypertension, heart attack, stroke and diabetes. He wanted a way to change the culture of health and wellness within his church.
In partnership with the church auxiliary leaders and pastor, we created a summer nutrition education program that included presentations held at the church by health professionals, an interactive cooking demonstration and multimedia video presentations. We had tons of fun and developed a genuine relationship with the church congregation. There were about 50 people in the original FAITH program, and we truly impacted the entire local faith community as the message spread throughout the congregation and the social networks of the members.
Journey to Mayo Clinic
I continued to have a nice relationship with the church and continued to attend worship services there while I completed my medical school and residency training. I decided to pursue a cardiology fellowship, as it was a beautiful fusion of my passion for cutting-edge and innovative medicine and public health. I fell in love with Mayo Clinic and its resounding value that "the needs of the patient come first." I was elated to be accepted into the fellowship program.
"Our program has sparked healthy lifestyle practices among our participants, but it's also changed their views and perspectives about participating in clinical research."
LaPrincess Brewer, M.D.
It was somewhat bittersweet to reveal the news of my life transition from Baltimore to the Midwest to the congregation. The church even threw me a very nice going-away party for my family and friends. The one common theme from the church members was to "not let FAITH go." They expressed to me through testimonials how the program had truly impacted their church and emphasized that the program would be of benefit to others. They wanted me to "spread the word" in a sense by sharing the program. I really took their encouragement to heart, and it has really motivated me to keep going and has brought me to this moment.
Opening doors in Rochester
When I arrived at Mayo Clinic, my advisers knew from the start that my interests included a focus on addressing cardiovascular health disparities given my prior work with FAITH and other community outreach programs during my residency training. Fortunately, they aligned me with key mentors, including Dr. Yvonne Romero, Dr. Sharonne Hayes and Dr. Joy Balls-Barry, who helped to forge relationships with several African-American pastors here in Rochester.
The pastors were privy to my work in Baltimore and wanted to bring this to their churches. In the fall of 2013, we held town hall meetings with several churches in Rochester. After much trust-building and mutual understanding, we decided to alter the focus of the program from chronic disease prevention to heart disease prevention, given the needs of this community and my expertise in cardiology.
The approach we use for conducting research is unique and is called community-based participatory research. This approach aligns well with Mayo Clinic's model of patient care, as it emphasizes that the needs of the community come first. We see the community as partners at every phase of the research process to meet their needs.
Together, we have forged a powerful relationship that has truly blossomed into a communitywide initiative. Our program has sparked healthy lifestyle practices among our participants, but it's also changed their views and perspectives about participating in clinical research.
Building trust and relationships
My first meetings with the Rochester African-American church community were not always easy but were extremely revealing of my purpose in partnering with this endearing, yet somewhat marginalized population. They expressed the limited academic-community level partnerships with their churches and also questioned my intentions. That was something I totally did not expect. They truly challenged me, but I am so appreciative for our enlightening dialogues because I learned many lessons on how to better tailor my approach and be adaptable.
We broke much ground with the Rochester African-American community by building trust and relationships. Many viewed their participation in this research study ultimately as a form of social justice. They felt their participation in this study was giving back to future generations within the community. They saw our program in a way as Mayo giving back. It has been fulfilling and an honor to have the opportunity to grow personally and professionally through our work.
"The suggestion from the community to remix FAITH to harness mobile technology was something I never would have imagined. It shows the power of community partnerships and learning through listening."
LaPrincess Brewer, M.D.
We initially partnered with three churches in Rochester and have now doubled the number of churches in our expanded program to the Twin Cities in a relatively short time frame. All churches and study participants have provided us with exceptional input which has resulted in the evolution of our program from face-to-face, in-person sessions to an innovative mobile health (mHealth) intervention.
Harnessing technology for wider reach
As a study team, we learned that the churches wanted a way to share this information with their family and friends. The participants suggested that we revamp FAITH to include a digital component. We decided as a community and research team to develop a digital app. We often say: "FAITH. There's an app for that." The information we previously delivered during the face-to-face sessions has been translated to the app for participants to share with others, and to have as a resource and tool to foster healthy lifestyle change.
The suggestion from the community to remix FAITH to harness mobile technology was something I never would have imagined. It shows the power of community partnerships and learning through listening.
In its current form, FAITH is easily adaptable and can be easily distributed and tailored toward any community. It would be my dream for it to be a national initiative to protect heart health in underserved populations. I am extremely grateful to lead this program as a junior staff (faculty) member because it has helped me to realize my potential. It has further inspired me to be a go-getter to take my research to the next level.
It all has been fueled by the needs of the community and patients I serve.
HELPFUL LINKS
- Learn more about heart disease and heart health disparities.
- Read about Cardiovascular Medicine at Mayo Clinic.
- Explore Mayo Clinic's Rochester campus.
- Request an appointment.