When Alice Alimurung was diagnosed with a rare and life-threatening tumor, she embarked on a hunt for a surgeon with enough expertise to remove the mass. The search led Alice from the Philippines to Minnesota and Mayo Clinic, where she found an experienced surgical team that saved her life.
For more than 15 years, Alice 'Peachie' Sacasas Alimurung knew she had a rare tumor next to her heart. Physicians told Alice, who lives in Manila, Philippines, that the tumor couldn't be surgically removed. Despite that, she was able to live a normal life as she raised her children. Then in March 2018, Alice woke up in the middle of the night and feared she was having a heart attack.
"It felt like there was a 200-pound gorilla on my chest," Alice says.
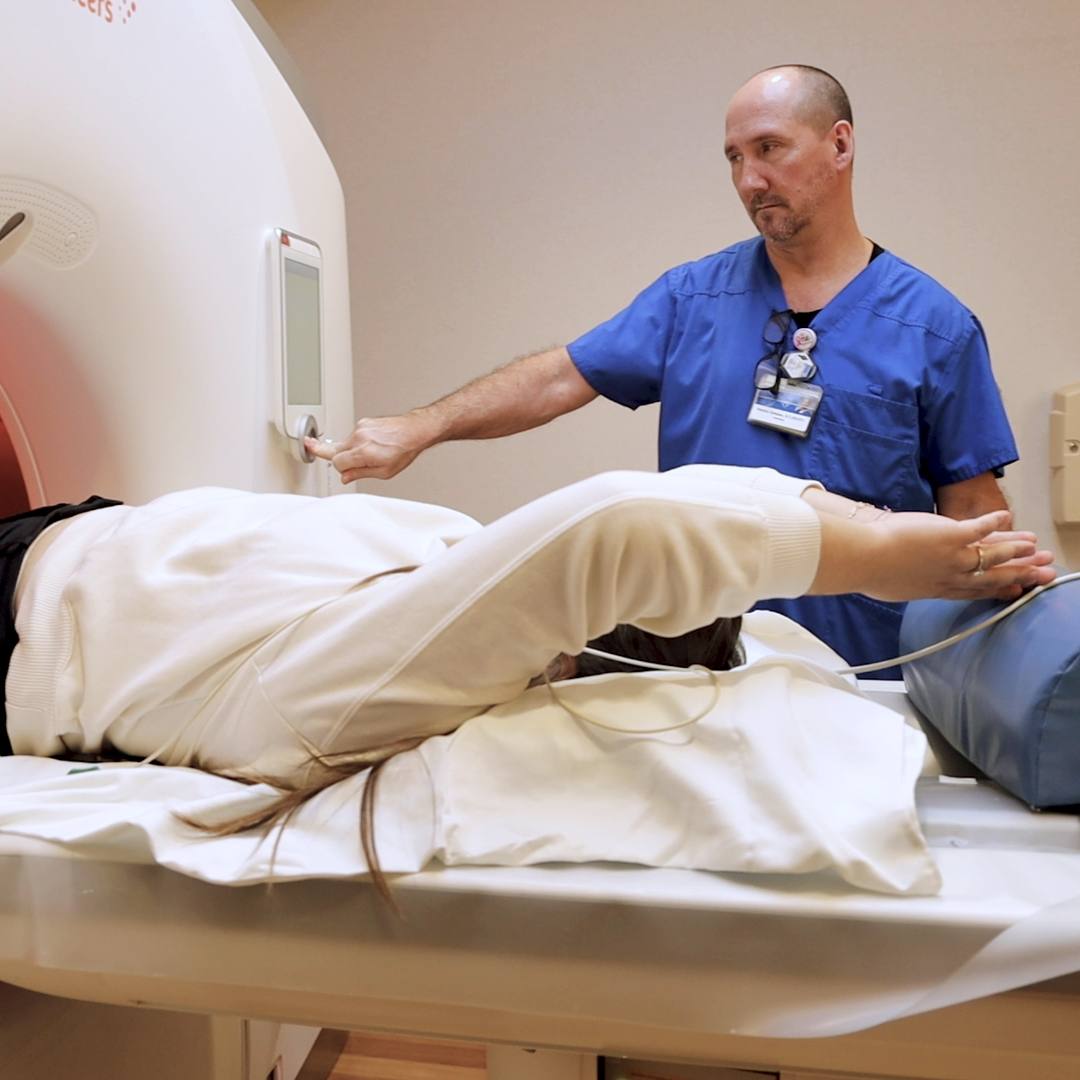
When Alice got out of bed and walked around, the feeling subsided. But the next day, she had an echocardiogram, followed by an MRI and CT scan. They revealed that Alice's tumor had grown substantially. It had spread into her vena cava, the major blood vessel that brings blood into the heart, and it was pressing against her heart. The scans also revealed the nature of the tumor, which Alice hadn't known before: mediastinal paraganglioma.
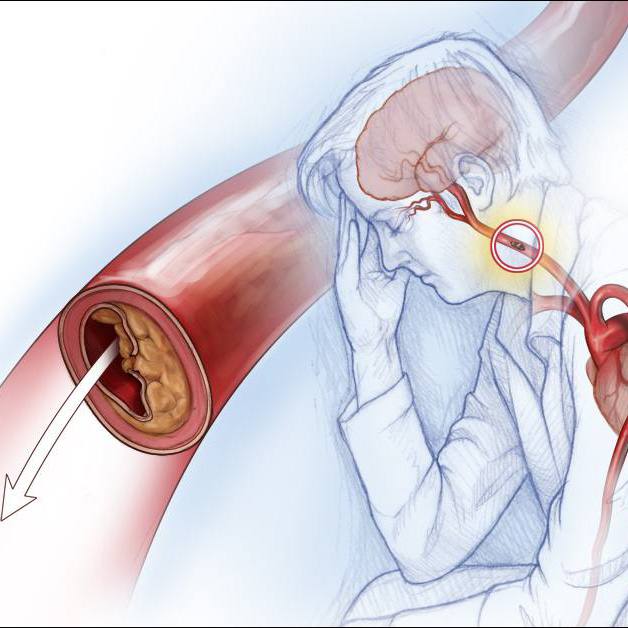
A rare tumor that generally grows within the vascular tissues near the heart, major blood vessels and esophagus, mediastinal paraganglioma has been reported only 150 times in medical literature. In some cases, the tumor can become cancerous. Treatment for mediastinal paraganglioma is surgical removal, when possible.
The discovery that Alice's tumor was invading vital cardiac structures set off an urgent, international search for a surgical team with expertise to treat her.
"I was really praying about it, asking for God to guide us. We were so desperate about this," Alice says. "We finally found Mayo Clinic in Rochester."
Since 1973, Mayo Clinic surgeons have operated on 14 patients with tumors like Alice's. Mayo Clinic also offered Alice the opportunity to be cared for by a multidisciplinary surgical team, including Hartzell Schaff, M.D., in Cardiovascular Surgery and Stephen Cassivi, M.D., in Thoracic Surgery.
"Dr. Schaff and Dr. Cassivi, they were both godsent to me," Alice says. "When we found them, it was no doubt an answered prayer."
From innocuous to dangerous
Alice's tumor was discovered in 2004 during an MRI to check for the source of back pain. At that time, the tumor was about 2 centimeters in diameter. Alice's physicians believed it was related to tuberculosis. She was prescribed antibiotics. In 2006, a scan revealed the mass had not grown. But in 2010, a CT scan showed that it had.
"I wasn't really dwelling on it because there were no symptoms," Alice says.
That changed in 2017 when Alice's heart began beating too fast. On the treadmill, her heart rate skyrocketed. Alice took beta blockers to control her heart rate, but her heart continued to beat rapidly. On a sightseeing trip in December 2017, she felt out of breath and exhausted.
"I realized there was something wrong, but I still didn't mind it until that dreadful evening in March."
Alice Alimurung
"I realized there was something wrong, but I still didn't mind it until that dreadful evening in March," Alice says.
Following her nighttime cardiac episode and the ensuing diagnosis, Alice's symptoms became constant and painful. With the help of her local medical team, Alice and her husband, Benjamin Alimurung — who is a cardiologist in the Philippines and understood his wife's precarious condition — contacted one medical facility after another. Their efforts to find a surgical team that could operate on Alice were met with rejection, which amplified Alice's physical distress.
"The way that it was going, no one wanted to give me health care," Alice says. "I remember telling my husband, 'Just let me die a natural death.' But my husband said, 'Oh no, as long as I'm alive, I will give you the best health care.'"
Alice's search eventually led her back to a hospital in Manila: St. Luke's Medical Center. While surgeons at St. Luke's were not equipped to remove the tumor, they connected Alice with a place that could: Mayo Clinic.
As a member of Mayo Clinic Care Network, St. Luke's physicians opened a line of communication between Alice and Mayo Clinic. Alice's case was brought before Dr. Schaff, who reviewed it with his team and recommended tumor removal.
Preparation and collaboration
Alice and Benjamin flew to Mayo Clinic's Rochester campus, and on July 1, 2018, Dr. Schaff began preparations to remove the tumor.
"It was complicated to remove because of its size, vascularity and its location," Dr. Schaff says. "It was situated above the left atrium and had compressed her superior vena cava."
By the time Alice reached Mayo Clinic, the mass was about the size of an orange.
"These are very vascular tumors. They have a lot of blood supply to and from the tumor," Dr. Cassivi says. "And hers was sitting amidst all of the vessels on the top of the heart, and you have not just the large blood vessels moving in and out of the heart, but the small blood vessels that feed the heart muscle itself."
To prepare for the surgery, Alice's team had the Mayo Clinic 3D Printing Lab make two models of the tumor, heart and surrounding blood vessels. The first model could be broken down to demonstrate how the varying structures fit together. The second model was transparent and showed how the blood flowed through Alice's vessels. Even with this preparation, Alice's surgical team couldn't completely predict the extreme vascularity of the tumor.
"When we started to remove it during the initial operation, the bleeding got to the point where we felt like if we did resect anymore, we wouldn't be able to control the bleeding," Dr. Schaff says. "So we stopped the operation with the idea of asking our colleagues in Interventional Radiology to occlude the feeding vessels to the tumor."
While it's unusual to stop an operation midway through a procedure, in Alice's case, removing any more of her tumor would have put her life at risk, Dr. Schaff says.
"I woke up in between surgeries knowing something was up. It was a surprise, indeed, a lifesaving change in plan."
Alice Alimurung
Under the direction of Christopher Reisenauer, M.D., a Mayo Clinic interventional radiologist, several of the fine arteries feeding Alice's tumor were blocked. Next, a team of interventional cardiologists, including Rajiv Gulati, M.D., Ph.D., Donald Hagler, M.D. and Patricia Best, M.D., stepped in. The team used tiny coils to selectively embolize, or block, some of the branches of the heart's coronary arteries that fed the tumor. The coronary arteries that supplied blood to her heart were preserved.
After these procedures, Alice was taken to the Cardiac Intensive Care Unit, where she was awakened from sedation.
"I woke up in between surgeries knowing something was up," Alice says. "It was a surprise, indeed, a lifesaving change in plan."
When her team considered Alice strong enough for the final stage of the operation, she was put back to sleep.
"We took the tumor out, and bleeding was less of a problem because of what the teams in Radiology and Cardiology did," Dr. Schaff says. After removing the tumor, Dr. Schaff reconstructed Alice's vena cava.
When Alice began regaining consciousness following that surgery, the news was good.
"When I saw Dr. Schaff, he was happy to see how well I was recovering," Alice says. "He said, 'You really are one for the books.'"
 Smooth recovery, ideal outcome
Smooth recovery, ideal outcome
While recovering in the hospital, Alice says she was comforted by the constant support of her care team.
"The ICU nurses are the best ever," Alice says. "They were extremely caring and gentle."
Alice remained in the hospital for nearly three weeks before she was discharged to nearby housing, where she stayed for another week. Four weeks after her operation, Alice received the go-ahead from Drs. Schaff and Cassivi to fly back to Manila. Once home, Alice began cardiac rehabilitation. In November 2018, Alice returned to the gym, where she walks on the treadmill and lifts light weights.
Alice will continue to be followed by her cardiology team at St. Luke's, and she'll have checkups with her Mayo Clinic team, as needed, using telecommunications equipment.
"We can participate through video conference and virtual visits, and then can provide meaningful, long-term follow up for her without her necessarily having to make the trip," Dr. Cassivi says.
"When I saw Dr. Schaff, he was happy to see how well I was recovering. He said, 'You really are one for the books.'"
Alice Alimurung
Although there is a possibility Alice's tumor could return, her team is optimistic that it's not going to come back. "We hope the operation is curative," Dr. Schaff says.
The ability of the many members of Alice's care team to work in harmony with the goal of saving Alice's life was key to her successful results, according to Dr. Cassivi.
"It really was a coming together of so many different specialists to provide their expertise," he says, "which brings us to a really unbelievable outcome that I don't think could happen in many other places."
HELPFUL LINKS
- Learn more about paraganglioma tumors.
- Check out Cardiovascular Surgery and Thoracic Surgery at Mayo Clinic.
- Talk with others about heart and blood health on Mayo Clinic Connect.
- Explore Mayo Clinic.
- Request an appointment.