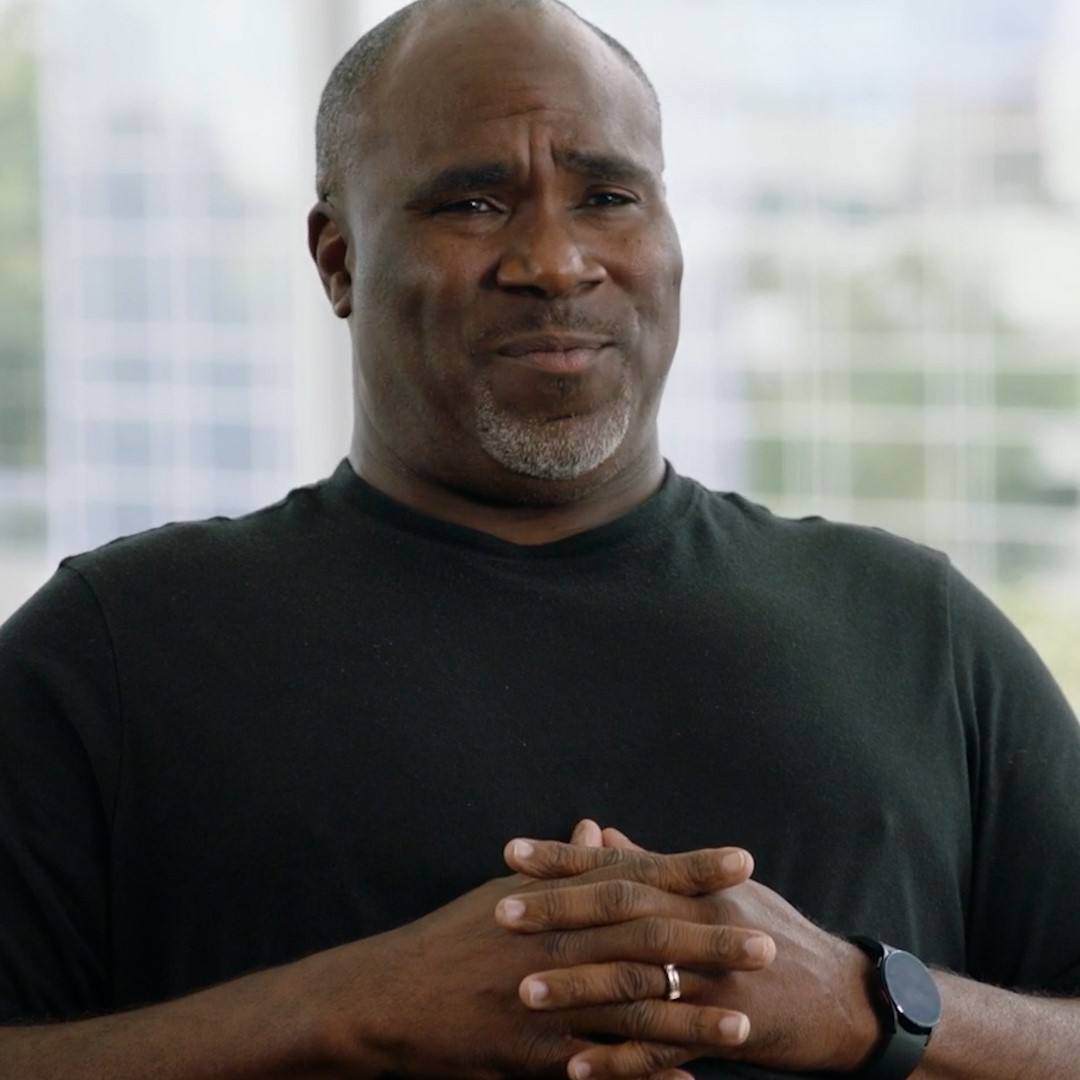
When Scott Stewart learned he had a rare neuroendocrine tumor, the journey ahead of him looked frightening and difficult. But with steadfast support from an interdisciplinary Mayo Clinic team, Scott now takes comfort in knowing that some of the best physicians in the world are walking the path with him.
These days, Scott Stewart spends his time on activities that make him happy. Using his hands to construct beautiful homes, spending time with his wife, Stephanie, exercising and strengthening his body, and fishing off his bass boat provide joy to the 54-year-old cancer survivor. Scott, who's lived with a rare neuroendocrine cancer for more than 11 years, appreciates the impermanence of life more than most.
"A lot of cancer patients figure out you'd better do some things in life that make you happy because you only have one shot at it," says Scott, who lives in Olathe, Kansas. "Making money is good. But you can't take it to the grave with you, so you'd better enjoy some stuff while you're here."
Scott's ability to seize the day while remaining attuned to the fact that his cancer will likely recur is mindfulness fostered by support from a team of Mayo Clinic physicians whose expert care has guided him through years of treatment.
"They've given me hope and confidence in what we've done, and it helps me remain optimistic," Scott says "Mayo helps me keep my optimism high that we can find a solution for whatever is thrown at me."
Extreme hunger signals serious illness
Scott's medical concerns began when he was a teen, and he became extremely sensitive to hunger. "I remember always having to eat all the time," he says. "If I didn't eat every couple of hours, I would start getting lightheaded. I just wouldn't feel good, and it got progressively worse."
Scott attributed his appetite issues to an active lifestyle and physically demanding jobs. But as he aged, he sought medical care from a local endocrinologist. His doctor found that Scott had low blood sugar, and worked to regulate it and the symptoms it caused. But in late 2007, Scott's body sent a clear message something was drastically wrong.
"Basically, I just went to sleep, and I didn't wake up," Scott says. His teenage son called 911. "The next thing I know there were paramedics around me. They'd put some glucose in me, and the lights turned back on."
In the emergency department, Scott's physicians couldn't identify the source of his blackout. But a short while later, after he blacked out again, a different physician ordered an abdominal CT scan. "That is when they discovered these tumors," Scott says. "My doctor knew someone at Mayo, and he put in a phone call. They were like, 'How quick can you get him up here?'"
"My kids were young, and I had a lot of life left in me."
Scott Stewart
Five days later, Scott and Stephanie drove 450-miles to Mayo Clinic in Rochester, where a team of specialists from Endocrinology, Interventional Radiology and General Surgery coalesced around him.
They discovered Scott had a rare type of cancerous neuroendocrine tumor that forms from the islet cells of the pancreas. "Islet cells are small, scattered cells through the pancreas, and their normal job is to produce hormones such as insulin," says Scott's Mayo Clinic oncologist, Timothy Hobday, M.D., in Medical Oncology. "When they become cancerous, they can produce an excess amount of a hormone."
In Scott's case, the excess hormone was insulin, and it caused his blood sugar to drop. When blood sugar dips too low, people feel lightheaded, become sweaty and can pass out. "Especially if they've gone without eating for a couple of hours or have exercised, it can be life-threatening if they don't have access to glucose," Dr. Hobday says.
When Scott's cancer was discovered, his pancreas and liver were riddled with tumors. Learning he had an advanced case of a rare and often incurable cancer was difficult to process. "When you find out, you go through a range of emotions," Scott says. "Some people only live five years after getting this. You really don't know. My kids were young, and I had a lot of life left in me."
Hard truths and extensive treatments
As hard as it was for Scott to hear, learning the nature of his condition was an important part of managing the disease. "It makes all the difference in the world to have people who give you the truth and give you information," he says. "You need to try to get a plan, even within yourself, so you can prepare for what you've got to do."
The first part of Scott's treatment involved attempts to control his symptoms with medications and an interventional radiology procedure to rapidly kill some of the cells and lower insulin production. After those initial steps, Scott had surgery to remove the tumors occupying much of his pancreas and liver.
"Most of the organs in our body, we can get by with less than the total complement," Dr. Hobday says. "Scott still has enough pancreas to perform regular hormone function and aid in the digestion that the pancreas performs, and he had enough liver left to function normally."
"Scott tolerated the treatment well, and it resulted in a significant improvement in quality of life, despite ongoing chemotherapy."
Timothy Hobday, M.D.
Following surgery, Scott's health improved for a time. But three years later, in early 2011, the symptoms of low blood sugar returned, and the cancer grew back in his liver. "At the time, I decided to put him on a relatively new kind of oral chemotherapy, which is a combination of two chemotherapy medications," Dr. Hobday says. "Thankfully, this very rapidly and very significantly reduced the total amount of his cancer by about 90% and got rid of all of his symptoms. Scott tolerated the treatment well, and it resulted in a significant improvement in quality of life, despite ongoing chemotherapy."
During the year Scott received chemotherapy, his Mayo team worked out the next phase of his treatment. Dr. Hobday enlisted the help of colleagues in the Department of Gastroenterology and Hepatology, and together they decided to offer Scott a liver transplant. "It's an unusual step, concluding he would be a good candidate for liver transplantation," Dr. Hobday says. "But the cancer was contained to his liver, and this is an approved, though uncommon, role for liver transplantation."
Although he chose a medical facility closer to home for his liver transplant, which took place in September 2012, Scott stayed in contact with Dr. Hobday. "He would just call me and make sure that someone was looking out for me," Scott says. "I don't know any other doctor that does that. Dr. Hobday really does look after my case, and things don't just slide through the cracks."
Reprieve and recurrence
After the transplant, Scott received routine follow-up care at home to check for liver rejection and cancer recurrence. For three years, Scott's test results, which he forwarded to Mayo, came back clear. But in summer 2015, a small mass was discovered in an abdominal lymph node near his liver. His Mayo Clinic team put their heads together to determine the best course of treatment. They decided to surgically remove the affected lymph nodes.
For another three years after that surgery, Scott's scans again were normal, but eventually he noticed his appetite changing. "I used to shrug it off, but I've been taught by Mayo that you do need to monitor these things because they could lead to something bigger," he says.
Scott's next blood test revealed his liver enzymes were up, and a CT scan was done. Although the scan appeared normal, Scott insisted the images be forwarded to Mayo. Within a few days, Dr. Hobday called Scott to tell him that a new tumor had developed in another abdominal lymph node near his liver.
"Again, his surgeon reviewed the situation carefully and tried to decide the best surgical approach and level of expertise needed." Dr. Hobday says. "It's remarkable that multiple surgeons of different subspecialties discussed his situation and all decided who would be the best equipped person to do the procedure. In this case, it was a liver transplant surgeon despite the fact that we hadn't performed his transplant here, and it wasn't a transplant surgery."
Personalized care breeds confidence
Since that surgery, Scott's scans haven't revealed any further signs of cancer. Given the nature of his illness, it is unlikely they will stay that way. But Scott doesn't dwell on the negative.
"My emphasis is on the confidence that I have now through the analysis that I get at Mayo Clinic," Scott says. "They look at enough of the angles that they have a very thorough understanding of what's going on, and I feel like they really give the answers. They're not necessarily all of the ones I want to hear, but I feel like they are the answers that are the truth."
Because Mayo Clinic physicians understand the value of teamwork, patients with rare illnesses like Scott receive the personalized, comprehensive care they require.
"This gentleman has not just lived, but thrived with this metastatic incurable cancer for now over 11½ years, and at this time, we don't have any sign of active cancer in him," Dr. Hobday says. "In Oncology, we see a lot of these cases from all over the world because they are referred to us. Ultimately, to take care of them, we have to have a smart team of people all working together. Every step of the way, multiple specialists discussed where we were and where we needed to go next. This is a remarkable example of the team care that you need to have to take optimal care of these patients."
HELPFUL LINKS
- Learn more about neuroendocrine tumors.
- Visit Mayo Clinic's Department of Oncology.
- Read about liver transplants.
- Connect with others talking about neuroendocrine tumors on Mayo Clinic Connect.
- Explore Mayo Clinic.
- Request an appointment.