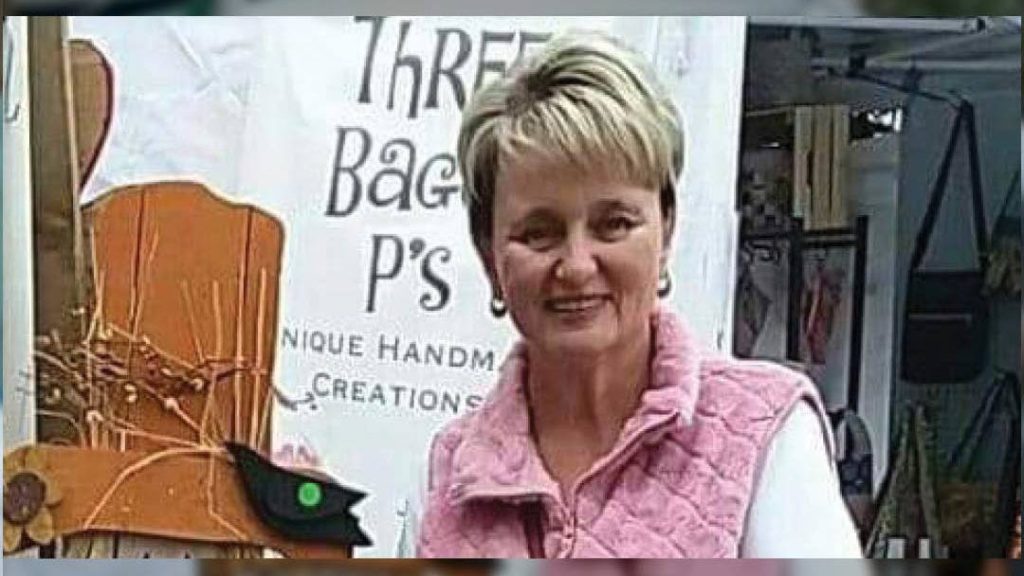
Belinda Purdy isn't the type of person who enjoys sitting on the sidelines. She and her family love to travel, swim, eat out and spend time outdoors. She's used to being on her feet all day and loves to walk 3 or 4 miles per day.
But in spring 2020, Belinda felt like she was watching the world go by as she sat still. The problem was debilitating pain in her hip and low back.
Pain brewing
Her troubles began when she lived in Colorado in 2015. She started having low back pain, and soon she couldn't stand pain-free for more than five minutes.
"I visited a nurse practitioner there and got a steroid injection and did therapy," says the 51-year-old Black River Falls, Wisconsin, resident. "I didn't think much about it again."
For Belinda, the pain relief was short-lived. While moving to Wisconsin in 2018, the hip pain returned. This time, it included pain extending down her right leg.
"It started as pain in my right hip. I tried to stretch and keep walking. I thought it would go away," says Belinda. "Moms can be pretty stoic, and I muddled through it."
Over time, the pain became more intense and started to affect her daily activities.
"I needed to sit on a chair while cooking because I couldn't stand next to my stove. I could hardly walk to my car because I was in agony," says Belinda, who previously worked as a nurse. "On a scale of 1 to 10, my pain was like an 11."
Steps to relief
By early 2020, Belinda was increasingly frustrated by the pain and began to worry that she would spend the rest of her life sitting in a chair.
Her family convinced her to make an appointment with Michael Stark, D.O., her primary care provider at Mayo Clinic Health System in Tomah, Wisconsin. After examining her, Dr. Stark referred Belinda to physical therapy. Unfortunately, it didn't provide pain relief like it had before.
"I was limping after therapy and could not walk," says Belinda. Previously, she was walking 3 to 4 miles per day but now was unable to walk from the parking lot into the hospital. "I had to sit halfway there and rest."
Finding the cause
Dr. Stark referred Belinda to Navid Khezri, M.D., a Mayo Clinic Health System neurosurgeon, who arranged for advanced imaging of her spine prior to the appointment. The scans revealed the cause of her pain: forward slip of the last lumbar spine bone over the tail bone. This also is called "L5/S1 spondylolisthesis."
The imaging also revealed chronic fractures of the two supportive bony pillars on the backside of the L5 vertebrae called pars. A bone density assessment showed that Belinda also had osteoporosis.
Belinda knew she had scoliosis at a young age, but she was surprised to learn of the fractures and the extent of her osteoporosis.
"Ms. Purdy had pars fractures on both sides of her L5 vertebrae. Over time, the chronic fractures along with the normal wear and tear of life and aging led to the loss of structural integrity at L5/S1. This resulted in her L5 slipping forward relative to her sacrum," says Dr. Khezri. "When this happens, the nerves that are located between the two bones get pinched. Nerve compression and the instability between L5 and S1 were the main sources of her pain."

Chronic pars fractures and defects are more common than people may expect, Dr. Khezri explains.
"It is common to have these defects in the pars, either because of an early fracture that never healed or a congenital problem," he says. "Over time, degeneration of the spine builds up. The bones begin to slip relative to each other and eventually end up becoming problematic. This is a well-known cause of back pain."
Surgical treatment
Dr. Khezri explained that surgery was the best option to stabilize the joint and relieve her pain.
"Back pain due to pars defect and bony slips tends to respond very well to surgery," he explained.
Belinda didn't hesitate.
"Dr. Khezri was very kind, warm and welcoming," she says. "I felt like I was in great hands."
Dr. Khezri performed a two-part procedure on her spine in June 2020. This included an anterior lumbar interbody fusion, also called ALIF, and a posterior minimally invasive pedicle screw fixation.
"Although there are different surgeries to address bony slips secondary to pars defects, ALIF with posterior support is considered the gold standard," he says.
During the first part, Dr. Khezri accessed Belinda's spine from the front, rather than her lower back. He removed the L5/S1 disc, which allowed him to push L5 back in alignment with the rest of the spine. He then placed a spacer cage between L5/S1.
The second part of the surgery was completed with two small incisions on her back. Additional screws and rods were inserted to fuse Belinda's L5 and S1 vertebrae. Both parts of the surgery were completed in one day.
Belinda's surgery went well. She spent two days in the hospital and then went home to recover.
Moving again
Belinda didn't waste any time before going for a walk, albeit slowly at first.
"I had sat for too long, so I started walking the day I came home from the hospital," says Belinda. "I walked up and down my driveway. Then every day, I walked a bit further."
She was sore and had some surgical pain at the beginning of her recovery. But she was thrilled that the debilitating back and hip pain was gone. In about four weeks, Belinda was walking up to 2 miles each day. Six months after surgery, she increased her walks to 4 miles per day and started swimming again.
Dr. Khezri was not surprised by her desire to get moving and her quick return to her active life.
"This problem had ground her life to a halt and put an end to her lifestyle as she knew it," he says. "She was very motivated and passionate about being active again. She was compliant with her surgical restrictions and did very well. This is exactly the outcome we were hoping for her."
Belinda is enthusiastic about her surgery's success and her future.
"I am so excited that I don't have that pain anymore and grateful for everyone who touched me during my care," Belinda says. "I am forever grateful and feel like I got my life back."
This story published first on the Mayo Clinic Health System Hometown Health site.
Related Articles







